
1987 Texas flood survivors reflect on nearly 40 years of loss, faith and hope
For those affected by the Texas floods, the pain is overwhelming and the road to healing is uncertain.
Watch CBS News

For those affected by the Texas floods, the pain is overwhelming and the road to healing is uncertain.

While there's still hope in the Hill Country that survivors are still out here, finding bodies at least offers some level of comfort to the families who have been waiting four agonizing days.

Even those not affiliated with an organization are eager to help give back to the community after devastating floods.

Amid criticism of budget cuts at NWS, Sen. Ted Cruz defended the agency, saying meteorologists did their job and were not short-staffed during the early morning hours of July Fourth.

Roads disappeared under rushing water. Homes and businesses were submerged as the Fourth of July weekend turned into a rescue mission.

For days before catastrophic floods left parts of Central Texas inundated, the National Weather Service was tracking the chance of rain.

President Trump said Sunday that he would have gone to Texas immediately but he would be "in their way."

Lt. Gov. Dan Patrick told CBS News Monday that the state could pay for storm sirens along the Guadalupe River.

Their expertise is exactly what officials say is needed to conduct these kinds of rescues.




For those affected by the Texas floods, the pain is overwhelming and the road to healing is uncertain.

While there's still hope in the Hill Country that survivors are still out here, finding bodies at least offers some level of comfort to the families who have been waiting four agonizing days.

Even those not affiliated with an organization are eager to help give back to the community after devastating floods.

Amid criticism of budget cuts at NWS, Sen. Ted Cruz defended the agency, saying meteorologists did their job and were not short-staffed during the early morning hours of July Fourth.

Roads disappeared under rushing water. Homes and businesses were submerged as the Fourth of July weekend turned into a rescue mission.

Their deaths were confirmed Saturday by St. Rita Catholic Community church.

A federal law enforcement source told CBS News that local police arrested eight people. The official said some of those apprehended were wearing body armor.

Whitney Slough said her husband and their two daughters were snorkeling about 20 feet from the beach when a small boat appeared along the shoreline.
Sometimes when life is at its worst, people are at their best. The last several days brought a deep heartache in this state, but also a deep love and persistence. Through the heat, the rain, and the unforgiving terrain our first responders have searched. Strangers. Neighbors. Texans have searched.

How do you even begin to cope with such heartbreaking loss? It's a question Richard Koons has been grappling with for nearly 40 years.

Along the Guadalupe River, volunteers are racing against time to find missing flood victims, with some bodies recovered by search dogs amid devastating floodwaters.

In the wake of the catastrophic Central Texas floods that have claimed the lives of more than 100 people, first responders and organizations from across the state have mobilized to join search efforts for those who remain missing.

Texas Republican State Rep. Jared Patterson and Democratic State Rep. Joe Moody have launched a bipartisan fundraising campaign with a goal of raising $150,000 to support affected families, first responders, and the broader community affected by the deadly flooding in Central Texas. Patterson discusses the tragedy’s impact and calls for improved emergency preparedness in future legislative sessions.
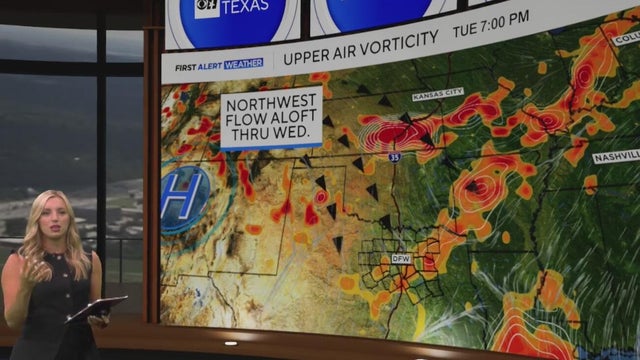
Spotty showers and storms will continue Tuesday and Wednesday before North Texas dries out Thursday.
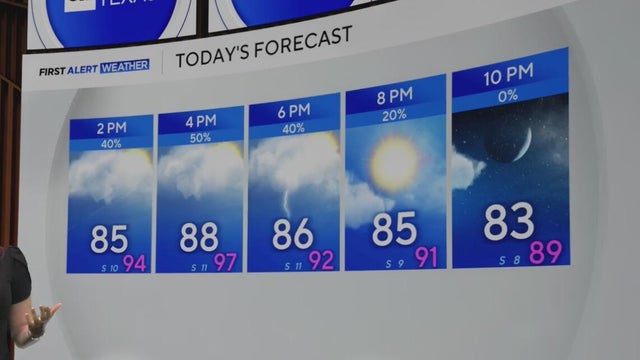
Spotty showers and storms will continue Tuesday and Wednesday before North Texas dries out Thursday.
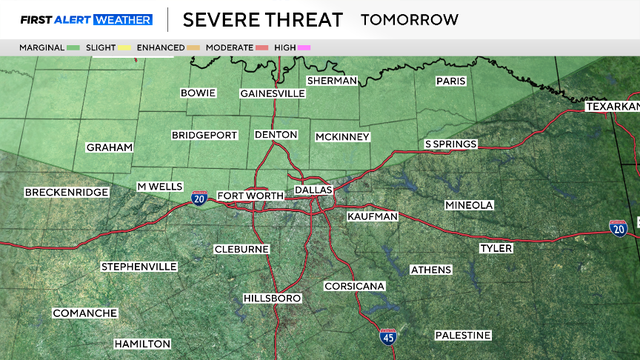
A Flood Watch is in effect for the area until 7 p.m. as an additional 2"-4" and isolated amounts up to 10" are possible.
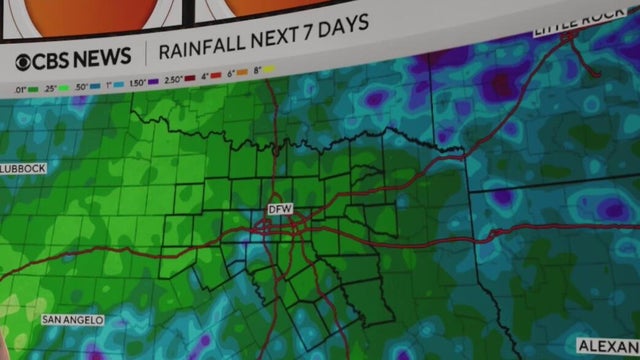
Over the next three days, showers and storms will move across parts of North Texas that may prompt a few flood watches and warnings.

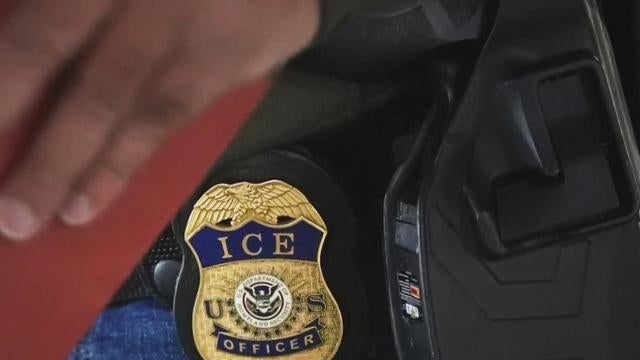
Two weeks ago, the Trump administration began carrying out its latest tactic aimed at fast-tracking deportations.

The detentions come on the heels of similar arrests earlier this week in immigration courts across the country.

Multiple sources have confirmed that at least a handful of people were arrested on the spot after their cases were dismissed in Dallas.

While illegal migrant crossings have dropped, immigration courts now have a historically high volume of cases

With the expansion of the 287(g) program, local and state officers will be able to enforce some immigration duties.
While the Trump administration says they're only targeting criminals for deportation, those words have done little to comfort some immigrants
A few weeks into his second term, President Donald Trump has issued dozens of executive orders.

Two faith leaders view border politics through different lenses.

Many Texas law enforcement officials say they are feeling positive as Donald Trump re-enters the White House for a second term.

The Cowboys, Texans and the NFL are helping those in need as recovery continues after devastating floods ravaged the Hill Country.

Turpin, 28, was booked into the Collin County jail for possession of marijuana and unlawful carrying of weapon, records show.

Ben McLemore was found guilty by a Portland-area jury of raping a woman at a party attended by many of his then-Portland Trail Blazer teammates.

Aziaha James scored 20 of her 28 points in the first half, Paige Bueckers added 23 and the Dallas Wings started four rookies in a 98-89 victory over the Phoenix Mercury.

The Dallas Mavericks have signed No. 1 overall draft pick Cooper Flagg to his four-year rookie contract.
Texas does BBQ best so we took the Cadillac to Loop 9. Don’t miss out on all the traditional favorites and some with a twist. Eat See Play is sponsored by Metroplex Cadillac Dealers.

When that fine dining craving hits, jump in the Cadillac and head to The Landmark Prime Rib. Let your dinner take center stage as your meal is prepared in their vintage dining cart. Eat See Play is sponsored by Metroplex Cadillac Dealers.

Ready to get your golf on? Throw your clubs in the Cadillac and head to Tiger Woods's new putt-putt playground, Popstroke. Eat See Play is sponsored by Metroplex Cadillac Dealers.

Which hue looks best on you? We took the Cadillac to the Color Analysis Queen to see which shades make us shine. Eat See Play is sponsored by Metroplex Cadillac Dealers.

Eat. See. Play: Meow Wolf

Eat See Play at Rooftop Cinema Club

Eat See Play: Glazed Ceramic Studio

Eat See Play: Permanent Jewelry at Mod + Jo

Eat See Play: Dallas Silk Art

For those affected by the Texas floods, the pain is overwhelming and the road to healing is uncertain.

While there's still hope in the Hill Country that survivors are still out here, finding bodies at least offers some level of comfort to the families who have been waiting four agonizing days.

Even those not affiliated with an organization are eager to help give back to the community after devastating floods.

Amid criticism of budget cuts at NWS, Sen. Ted Cruz defended the agency, saying meteorologists did their job and were not short-staffed during the early morning hours of July Fourth.

Roads disappeared under rushing water. Homes and businesses were submerged as the Fourth of July weekend turned into a rescue mission.

For days before catastrophic floods left parts of Central Texas inundated, the National Weather Service was tracking the chance of rain.

Lt. Gov. Dan Patrick told CBS News Monday that the state could pay for storm sirens along the Guadalupe River.

Federal investigators are examining the role driver fatigue may have played in a deadly I-20 crash near Terrell over the weekend.
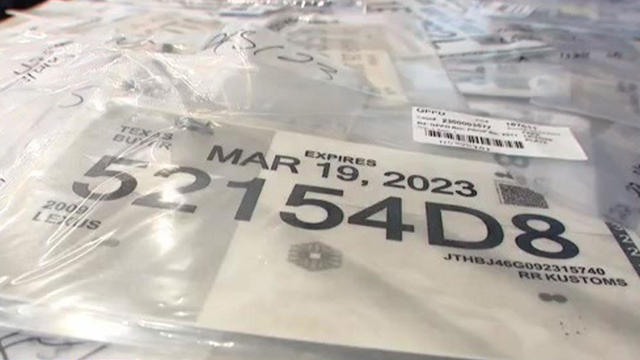
All temporary paper tags should be gone from Texas roads by Sept. 1.

The settlement resolves a wrongful death lawsuit filed by the father of Andre Craig, who died after a collision with a police vehicle in Fort Worth.

Texas Republican State Rep. Jared Patterson and Democratic State Rep. Joe Moody have launched a bipartisan fundraising campaign with a goal of raising $150,000 to support affected families, first responders, and the broader community affected by the deadly flooding in Central Texas. Patterson discusses the tragedy’s impact and calls for improved emergency preparedness in future legislative sessions.

President Trump said Sunday that he would have gone to Texas immediately but he would be "in their way."

The Trump administration said Monday it will soon revoke the legal immigration status of more than 70,000 immigrants from Honduras and Nicaragua.

The Trump administration is expected to send dozens of letters to countries that have not made a trade deal, warning them that higher tariffs could kick in next month.

All Texas Republicans in the House, along with Senators John Cornyn and Ted Cruz, voted for it. Democrats who serve in Congress voted against the measure and called it "one ugly bill."

At Fort Worth ISD's North Side High School, the sounds of an American sport on the field meet mariachi music in the stands.

With new foods, such as the "Drowning Taquitos" and the "Beso de Angel," Tony's Taco Shop owners say they don't take their success for granted.

Latinas in Tech DFW started back up last year after the pandemic. They have lots of opportunities for Latinas to network, connect, and learn new skills.
Anchor Ken Molestina shows us how he makes his Cuban coffee for the CBS News Texas newsroom.
Del Olmo, who has played golf his entire life, recalls how rare the sport was for people like him growing up in Mexico City.

Less than two days after Delta Air Lines offered $30,000 to each passenger on board the flight that crashed and flipped in Toronto on Monday afternoon, the company is facing its first two lawsuits in the incident — and they likely won't be the last.
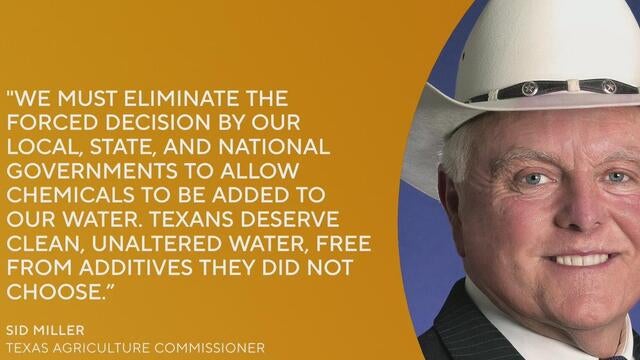
Texas Agricultural Commissioner Sid Miller is calling for a statewide ban on non-water additives, such as fluoride, in the public water system.

Last year, over 16 million vehicles drove on North Texas toll roads without paying, accumulating more than $69 million in unpaid tolls.

Activists are calling for a nationwide boycott of Target stores following the company's decision to roll back its diversity, equity and inclusion initiatives.

Discount store chain Target says it's joining rival Walmart and a number of other prominent American brands in scaling back corporate diversity, equity and inclusion initiatives.

It's therapy that doesn't exactly look like therapy: outdoors, alongside a horse. Across North Texas, the demand for it is soaring.

Scientists conducting medical research are facing an existential crisis: Layoffs and budget cuts pushed by President Trump that, they say, jeopardize finding a cure for cancer.

A Dallas mail carrier died Saturday after collapsing on his mail route on the first day of summer.

Pest control company Terminix used call data to determine which cities had the most bed bug-infested areas in the country.

Just weeks away from prom and graduation, 18-year-old Katie Rangel started feeling off.

They were already concerned about tariffs, but construction businesses in North Texas said they have new fears with the president's immigration crackdown.

The Texas Restaurant Association said 47% of Texas restaurant operators currently have job openings that are difficult to fill.

Plans to spruce up Frisco's historic downtown before next year's World Cup have business owners demanding help from the city to stay open.

A North Texas man who has made a fortune off of honey is turning to politics to save the creatures that made him rich.

The airport is projected to handle 100 million passengers by the end of this decade.

The Cowboys, Texans and the NFL are helping those in need as recovery continues after devastating floods ravaged the Hill Country.

Turpin, 28, was booked into the Collin County jail for possession of marijuana and unlawful carrying of weapon, records show.

Ben McLemore was found guilty by a Portland-area jury of raping a woman at a party attended by many of his then-Portland Trail Blazer teammates.

Aziaha James scored 20 of her 28 points in the first half, Paige Bueckers added 23 and the Dallas Wings started four rookies in a 98-89 victory over the Phoenix Mercury.

The Dallas Mavericks have signed No. 1 overall draft pick Cooper Flagg to his four-year rookie contract.

Sean "Diddy" Combs' lawyer says the music mogul got a standing ovation from fellow prisoners when he returned to the federal lockup in Brooklyn after the verdict.

Julian McMahon's last acting role before his death was playing the prime minister of Australia in Netflix's murder mystery series "The Residence."

Joey Chestnut is returning to the 2025 Nathan's Hot Dog Eating Contest. Here's how and when to watch.

Michael Madsen apparently went into cardiac arrest and was found unresponsive in his home in Malibu, California, on Thursday morning, according to his manager.

The multiplatform network owned by the once popular talk show host is facing financial struggles for which it finds its partner, Trinity Broadcasting Network, at fault.

A suspect was taken into custody after an attack on Pearl Street Mall in Boulder on June 1 in which there were 15 people and a dog who were victims. The suspect threw Molotov cocktails that burned some of the victims, who were part of a march for Israeli hostages.

The Neonatal Intensive Care Unit babies at Texas Health locations across North Texas celebrated Valentine's Day.

As Anthony Davis prepared for his debut game at the AAC, Dallas Mavericks fans took to the arena to protest the controversial trade.

CBS News Texas viewers got out and enjoyed the snow day on Thursday and send us all of their best photos. Take a look.

CBS News Texas captured the excitement and energy of the BMW Dallas Marathon Festival through photos.